· Mayank Kashyap · 8 min read
Gall bladder
According to Love and Bailey's "A Short Practice of Surgery", the gallbladder is a pear-shaped muscular sac located on the visceral surface of the liver that serves as a reservoir for bile. It plays a crucial role in the storage, concentration, and release of bile into the duodenum.
Introduction to the Gallbladder
According to Love and Bailey’s “A Short Practice of Surgery”, the gallbladder is a pear-shaped muscular sac located on the visceral surface of the liver that serves as a reservoir for bile. It plays a crucial role in the storage, concentration, and release of bile into the duodenum.
Clinical Significance
Most common site of biliary tract disease
Gallstone disease affects 10-15% of adult population
Cholecystectomy is one of the most common abdominal operations
Gallbladder cancer, though rare, has poor prognosis
Increasing incidence with age and obesity
Embryological Development
| Week | Development | Clinical Significance |
|---|---|---|
| 4th week | Hepatic diverticulum from ventral foregut | Origin of liver, gallbladder, and biliary tree |
| 5th week | Gallbladder primordium appears | Development of gallbladder and cystic duct |
| 12th week | Bile secretion begins | Functional development complete |
Surgical Anatomy of the Gallbladder
Gross Anatomy
| Feature | Description | Clinical Significance |
|---|---|---|
| Location | Gallbladder fossa on visceral surface of liver, segments IV and V | Anatomical relationship important for surgery |
| Dimensions | 7-10 cm long, 3 cm wide, capacity 30-50 mL | Distension in disease states |
| Parts | Fundus, body, infundibulum (Hartmann’s pouch), neck | Hartmann’s pouch common site for stone impaction |
| Relations | Anterior: Anterior abdominal wall Posterior: Transverse colon, duodenum Superior: Liver Inferior: Transverse colon | Important for understanding spread of inflammation |
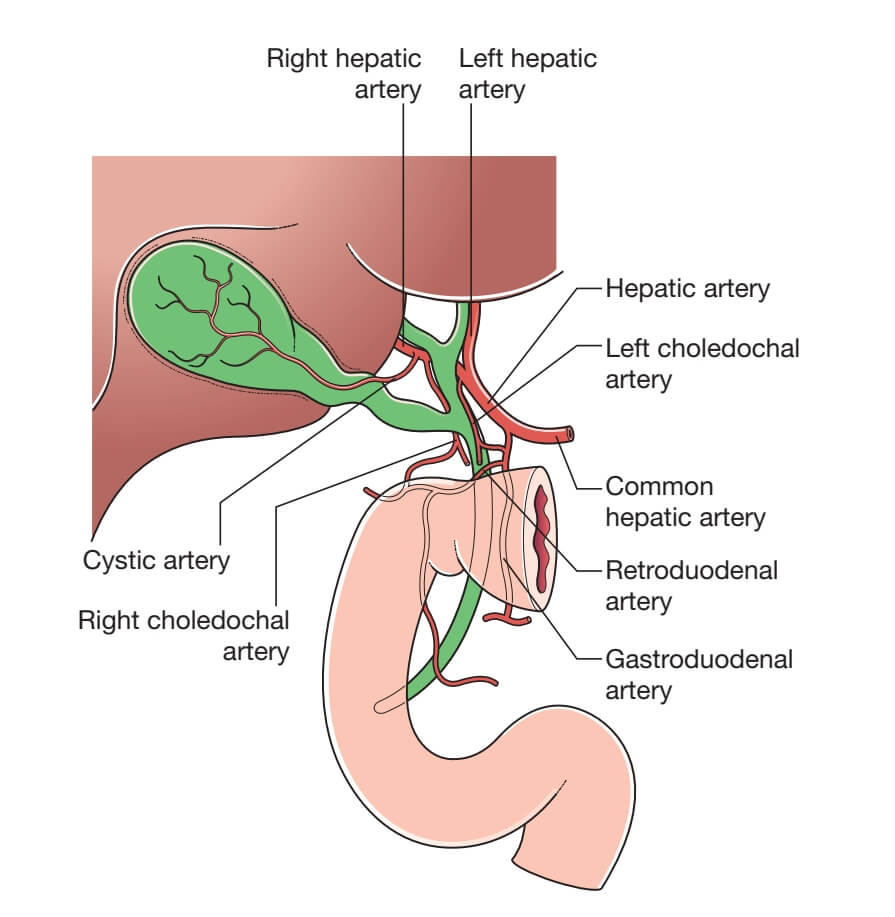
Blood Supply
| Vessel | Origin | Course | Surgical Importance |
|---|---|---|---|
| Cystic Artery | Usually from right hepatic artery (90%) | Through Calot’s triangle to gallbladder neck | Key structure in cholecystectomy, variations common |
| Cystic Vein | Drains directly to portal vein or right branch | Multiple small veins from gallbladder bed | Bleeding source during dissection |
| Arterial Variations | Multiple origins possible | From left hepatic, common hepatic, gastroduodenal arteries | Important to identify to avoid injury |
Calot’s Triangle
Boundaries:
Superior: Inferior surface of liver
Inferior: Cystic duct
Medial: Common hepatic duct
Contents: Cystic artery, cystic lymph node (of Lund), lymphatics
Surgical importance: Critical area for dissection during cholecystectomy
Critical view of safety: Clear identification of cystic duct and artery before division
Lymphatic Drainage
| Pathway | Nodes | Clinical Significance |
|---|---|---|
| Primary | Cystic node (Calot’s node) → hepatoduodenal ligament nodes | First echelon nodes for gallbladder cancer |
| Secondary | Pericholedochal nodes → celiac nodes → para-aortic nodes | Advanced drainage pathway |
| Additional | Direct drainage to liver, retropancreatic nodes | Explains unusual spread patterns |
Nerve Supply
| Nerve | Origin | Function |
|---|---|---|
| Sympathetic | T7-T9 via celiac plexus | Vasomotor, pain sensation (referred to right scapula) |
| Parasympathetic | Vagus nerve | Motor to gallbladder, stimulates contraction |
Histology
| Layer | Composition | Function |
|---|---|---|
| Mucosa | Columnar epithelium with microvilli, Rokitansky-Aschoff sinuses | Absorption and concentration of bile |
| Muscularis | Smooth muscle fibers in circular, longitudinal, oblique directions | Gallbladder contraction |
| Perimuscular | Connective tissue with vessels, nerves | Support and nutrition |
| Serosa | Visceral peritoneum (except liver attachment) | Covering and protection |
Gallbladder Physiology
Bile Composition
| Component | Concentration | Function |
|---|---|---|
| Bile Salts | 50-60% of solids | Emulsification of fats, cholesterol solubilization |
| Phospholipids | 20-30% of solids | Form mixed micelles with bile salts |
| Cholesterol | 3-5% of solids | Elimination of excess cholesterol |
| Bilirubin | 2-3% of solids | Excretion of heme breakdown products |
| Electrolytes | Similar to plasma | Maintain osmotic balance |
Gallbladder Functions
| Function | Mechanism | Capacity |
|---|---|---|
| Bile Storage | Reservoir function between meals | 30-50 mL |
| Bile Concentration | Active absorption of water and electrolytes | 5-10 fold concentration |
| Mucin Secretion | Protection of epithelium, lubrication | Variable |
| Acidification | Hydrogen ion secretion | pH 6.5-7.0 (from hepatic bile pH 7.5-8.2) |
Gallbladder Emptying
| Stimulus | Mediator | Effect |
|---|---|---|
| Food (especially fat) | Cholecystokinin (CCK) | Strong gallbladder contraction, sphincter of Oddi relaxation |
| Vagal Stimulation | Acetylcholine | Moderate contraction |
| Other Hormones | Motilin, gastrin | Mild contraction |
Enterohepatic Circulation
95% of bile salts reabsorbed in terminal ileum
Portal venous return to liver
Resecretion into bile (6-8 cycles/day)
Liver synthesizes 0.2-0.6 g/day to replace fecal losses
Investigations for Gallbladder Disease
Imaging Modalities
| Investigation | Indications | Findings | Sensitivity/Specificity |
|---|---|---|---|
| Ultrasound (USG) | First-line for suspected gallbladder disease | Stones, wall thickening, pericholecystic fluid, sonographic Murphy’s sign | 95% for stones, 80% for acute cholecystitis |
| CT Scan | Complicated cholecystitis, malignancy, unclear diagnosis | Stones (60-75%), inflammation, complications, lymph nodes | Good for complications, poor for uncomplicated stones |
| MRCP | Biliary anatomy, choledocholithiasis, biliary strictures | Detailed biliary tree anatomy, stones, tumors | 95% for bile duct stones, excellent anatomical detail |
| HIDA Scan | Suspected acute cholecystitis, biliary dyskinesia | Non-visualization of gallbladder in acute cholecystitis | 95% sensitivity, 90% specificity for acute cholecystitis |
| ERCP | Therapeutic for choledocholithiasis, biliary obstruction | Direct visualization, stone extraction, stenting | Gold standard for bile duct intervention |
Laboratory Investigations
| Test | Normal Range | Significance in Gallbladder Disease |
|---|---|---|
| Total Bilirubin | 0.2-1.2 mg/dL | Elevated in biliary obstruction |
| Alkaline Phosphatase (ALP) | 40-120 U/L | Elevated in biliary obstruction (early marker) |
| Gamma-Glutamyl Transferase (GGT) | 8-61 U/L | Elevated in biliary disease, more specific than ALP |
| ALT/AST | 7-56 U/L / 10-40 U/L | Mild elevation in biliary obstruction |
| Amylase/Lipase | 30-110 U/L / 7-60 U/L | Elevated in gallstone pancreatitis |
| White Blood Cell Count | 4,000-11,000/μL | Elevated in acute cholecystitis |
Sonographic Criteria for Gallbladder Disease
| Condition | Major Criteria | Minor Criteria |
|---|---|---|
| Acute Cholecystitis | Gallstones, sonographic Murphy sign, wall thickening >3mm | Pericholecystic fluid, gallbladder distension >8cm x 4cm |
| Chronic Cholecystitis | Gallstones, contracted gallbladder, wall thickening | Sludge, porcelain gallbladder |
| Gallbladder Polyps | Echogenic foci attached to wall, no acoustic shadowing | Size >10mm, solitary, sessile morphology |
Gallstone Disease (Cholelithiasis)
Types of Gallstones
| Type | Composition | Incidence | Risk Factors | Radiology |
|---|---|---|---|---|
| Cholesterol Stones | >70% cholesterol, with calcium salts, mucin | 80% in Western countries | Female, forty, fertile, fat, fair (5 F’s), rapid weight loss | Radiolucent (10-20% radio-opaque) |
| Pigment Stones | Calcium bilirubinate, <20% cholesterol | 20% in West, more common in Asia | Hemolytic anemia, cirrhosis, biliary infection, ileal disease | Radiolucent |
| Mixed Stones | 30-70% cholesterol with calcium salts | Most common overall | Combination of cholesterol and pigment stone risk factors | Often radio-opaque |
Pathogenesis of Cholesterol Stones
| Mechanism | Pathophysiology | Clinical Correlation |
|---|---|---|
| Cholesterol Supersaturation | Excess cholesterol secretion relative to bile salts and phospholipids | Obesity, high cholesterol diet, clofibrate therapy |
| Nucleation Factors | Mucin, calcium salts, proteins promote crystal formation | Gallbladder hypomotility, pregnancy |
| Gallbladder Hypomotility | Stasis allows crystal growth and stone formation | TPN, fasting, pregnancy, diabetes, octreotide |
Clinical Presentation of Gallstones
| Presentation | Symptoms | Signs | Management |
|---|---|---|---|
| Asymptomatic | None (incidental finding) | None | Observation (prophylactic cholecystectomy in selected cases) |
| Biliary Colic | Episodic RUQ pain, postprandial, radiating to back/scapula | RUQ tenderness, no fever, normal labs | Elective cholecystectomy |
| Complicated Disease | Persistent pain, fever, jaundice, vomiting | Murphy’s sign, fever, jaundice, peritonism | Urgent intervention depending on complication |
Natural History of Gallstones
| Outcome | Annual Incidence | Cumulative Probability (20 years) |
|---|---|---|
| Remain Asymptomatic | 70-80% | 60-70% |
| Develop Symptoms | 1-4% | 20-30% |
| Develop Complications | 0.1-0.3% | 1-2% |
Cholecystitis and Complications
Types of Cholecystitis
| Type | Pathogenesis | Clinical Features | Management |
|---|---|---|---|
| Acute Calculous Cholecystitis | Stone impaction in cystic duct → distension, inflammation, ischemia | RUQ pain, fever, Murphy’s sign, leukocytosis | Antibiotics, cholecystectomy (early vs. delayed) |
| Acute Acalculous Cholecystitis | Ischemia, stasis, concentration of bile in critically ill patients | Critically ill patient, fever, RUQ pain, often subtle | Urgent cholecystectomy or percutaneous cholecystostomy |
| Chronic Cholecystitis | Recurrent inflammation from stones, mechanical irritation | Recurrent biliary colic, dyspepsia, fatty food intolerance | Elective cholecystectomy |
| Emphysematous Cholecystitis | Gas-forming organisms in gallbladder wall (clostridia, E. coli) | Severe toxicity, gas on imaging, higher perforation risk | Emergency cholecystectomy, broad-spectrum antibiotics |
Complications of Acute Cholecystitis
| Complication | Incidence | Clinical Features | Management |
|---|---|---|---|
| Gangrenous Cholecystitis | 2-30% of acute cases | Severe pain, high fever, marked leukocytosis, sepsis | Emergency cholecystectomy |
| Perforation | 3-10% of acute cases | Sudden pain relief then peritonitis, abscess formation | Emergency surgery, drainage, antibiotics |
| Empyema | 5-15% of acute cases | Toxic, high fever, palpable mass, marked leukocytosis | Emergency cholecystectomy, antibiotics |
| Cholecysto-enteric Fistula | 1-2% of chronic cases | Gallstone ileus, chronic diarrhea, pneumobilia | Fistula repair, cholecystectomy, bowel resection if obstructed |
| Mirizzi Syndrome | 0.1-0.7% of cholecystectomies | Jaundice, stone impacted in Hartmann’s pouch compressing CHD | Difficult dissection, may require biliary reconstruction |
Tokyo Guidelines for Acute Cholecystitis (2018)
| Grade | Criteria | Recommended Treatment |
|---|---|---|
| Grade I (Mild) | No organ dysfunction, mild gallbladder inflammation | Early laparoscopic cholecystectomy (<72 hours) |
| Grade II (Moderate) | WBC >18,000, palpable mass, duration >72h, marked local inflammation | Early cholecystectomy or initial medical treatment then delayed surgery |
| Grade III (Severe) | Organ dysfunction (cardiovascular, neurological, respiratory, etc.) | Medical treatment and organ support, delayed cholecystectomy or percutaneous drainage |
Gallbladder Cancer
Epidemiology and Risk Factors
| Factor | Relative Risk | Mechanism |
|---|---|---|
| Gallstones | 4-5 times | Chronic inflammation, bacterial degradation of bile salts |
| Porcelain Gallbladder | 10-50% develop cancer | Chronic inflammation, calcification of wall |
| Gallbladder Polyps | Variable (size dependent) | Adenoma-carcinoma sequence, especially >1 cm |
| Chronic Infection | Salmonella typhi (6-8 times) | Chronic inflammation, bacterial enzymes |
| Anomalous Pancreaticobiliary Junction | 10-20% develop cancer | Pancreatic reflux, chronic irritation |
Pathological Types
| Type | Frequency | Features | Prognosis |
|---|---|---|---|
| Adenocarcinoma | 85-90% | Intestinal or biliary type, often scirrhous | Poor (5-year survival 5-10%) |
| Squamous Cell Carcinoma | 2-3% | Metaplasia of epithelium, aggressive | Very poor |
| Adenosquamous Carcinoma | 1-2% | Mixed glandular and squamous elements | Poor |
| Other (sarcoma, lymphoma) | Rare | Various patterns | Variable |
Staging of Gallbladder Cancer (AJCC 8th Edition)
| Stage | T | N | M | 5-year Survival |
|---|---|---|---|---|
| 0 | Tis | N0 | M0 | >80% |
| I | T1 | N0 | M0 | 50-60% |
| II | T2 | N0 | M0 | 20-30% |
| IIIA | T3 | N0 | M0 | 10-15% |
| IIIB | T1-3 | N1 | M0 | 5-10% |
| IVA | T4 | N0-1 | M0 | <5% |
| IVB | Any T | N2 | M0 or M1 | <2% |
Treatment Approaches
| Stage | Surgical Treatment | Adjuvant Therapy |
|---|---|---|
| T1a (incidental) | Simple cholecystectomy | None |
| T1b-T3 | Extended cholecystectomy with liver resection (segments IVb/V) and lymphadenectomy | Chemotherapy (gemcitabine/cisplatin), consider radiotherapy |
| T4 or N2 | Palliative procedures (biliary drainage, bypass) | Palliative chemotherapy, best supportive care |
Surgical Management of Gallbladder Disease
Cholecystectomy Techniques
| Procedure | Indications | Advantages | Disadvantages |
|---|---|---|---|
| Laparoscopic Cholecystectomy | Elective cases, uncomplicated acute cholecystitis | Less pain, faster recovery, better cosmesis | Learning curve, bile duct injury risk |
| Open Cholecystectomy | Complicated cases, conversion from laparoscopic, surgeon preference | Better visualization, tactile feedback, lower bile duct injury rate | More pain, longer recovery, larger scar |
| Single Incision Laparoscopic Surgery (SILS) | Selected elective cases | Better cosmesis, potentially less pain | Technically challenging, longer operating time |
| Robotic Cholecystectomy | Complex cases, teaching situations | 3D vision, tremor filtration, ergonomic | Cost, setup time, availability |
Critical View of Safety in Laparoscopic Cholecystectomy
Definition: A method to minimize bile duct injury by positive identification of structures
Three Criteria:
Clearance of fat and fibrous tissue from hepatocystic triangle
Separation of lower one-third of gallbladder from liver bed
Two and only two structures entering the gallbladder (cystic duct and artery)
Importance: Reduces major bile duct injury by 50-70%
Intraoperative Cholangiography
| Indication | Rationale | Findings |
|---|---|---|
| Routine | Anatomical mapping, detect unsuspected stones | Normal anatomy, unsuspected stones (5-10%) |
| Selective | Abnormal anatomy, elevated LFTs, pancreatitis, wide cystic duct | Anatomical variations, stones, injuries |
| Therapeutic | Stone extraction, sphincterotomy | Successful clearance or need for additional procedures |
Complications of Cholecystectomy
| Complication | Incidence | Risk Factors | Management |
|---|---|---|---|
| Bile Duct Injury | 0.3-0.5% (laparoscopic), 0.1-0.2% (open) | Acute inflammation, anatomical variations, surgeon experience | Intraoperative repair, hepaticojejunostomy, stenting |
| Bile Leak | 0.5-1% | Accessory ducts, cystic duct stump leak, liver bed leak | ERCP with sphincterotomy/stenting, drainage, reoperation |
| Bleeding | 0.5-1% | Portal hypertension, inflammation, vascular anomalies | Electrocautery, clips, sutures, angiographic embolization |
| Retained Stones | 1-2% | Multiple small stones, wide cystic duct, missed IOC | ERCP with sphincterotomy and stone extraction |
| Port Site Hernia | 0.5-1% | Large port sites, midline placement, obesity | Hernia repair |
Post-cholecystectomy Syndrome
| Cause | Frequency | Symptoms | Management |
|---|---|---|---|
| Biliary Causes | 10-15% | Retained stones, cystic duct stump, sphincter of Oddi dysfunction | ERCP, sphincterotomy, medical therapy |
| Non-biliary Causes | 85-90% | GERD, IBS, pancreatitis, other gastrointestinal disorders | Appropriate medical management |
| Extra-intestinal Causes | Rare | Cardiac, musculoskeletal, psychological | Specific to cause |
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Gallbladder and Biliary Tree in Love & Bailey’s textbook
Tokyo Guidelines 2018 for acute cholecystitis
Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Guidelines
American College of Surgeons Guidelines
World Society of Emergency Surgery Guidelines
Key Learning Points from Love & Bailey
“The gallbladder, though a small organ, presents significant surgical challenges. A thorough understanding of biliary anatomy, particularly the variations in cystic artery and duct anatomy, is essential for safe cholecystectomy. The critical view of safety remains the cornerstone of preventing bile duct injuries.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Always obtain a preoperative ultrasound for suspected gallbladder disease
Consider MRCP if complicated anatomy or suspected common bile duct stones
Follow Tokyo Guidelines for management of acute cholecystitis
Always achieve critical view of safety during cholecystectomy
Have a low threshold for conversion to open procedure in difficult cases
Consider gallbladder cancer in porcelain gallbladder or large polyps (>1 cm)
Multidisciplinary approach is essential for gallbladder cancer management
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog