· Mayank Kashyap · 6 min read
Inguinal hernia
An inguinal hernia is the protrusion of abdominal contents (usually intestine or omentum) through a weak point in the lower abdominal wall in the inguinal region, either through the inguinal canal or its posterior wall.
What is Inguinal hernia?
An inguinal hernia is the protrusion of abdominal contents (usually intestine or omentum) through a weak point in the lower abdominal wall in the inguinal region, either through the inguinal canal or its posterior wall.
Types
Direct Inguinal hernia
Indirect Inguinal hernia
Anatomy

L
Introduction to Inguinal Hernia
According to Love and Bailey’s “A Short Practice of Surgery”, a hernia is defined as the protrusion of a viscus or part of a viscus through its covering cavity wall. Inguinal hernia specifically refers to herniation through the inguinal canal.
Epidemiological Significance
Most common type of abdominal wall hernia (75% of all abdominal wall hernias)
Male to female ratio: 9:1
Lifetime risk: 27% in men, 3% in women
Right side more common than left (55% vs 35%, bilateral 10%)
Peak incidence: 0-5 years (congenital) and 40-70 years (acquired)
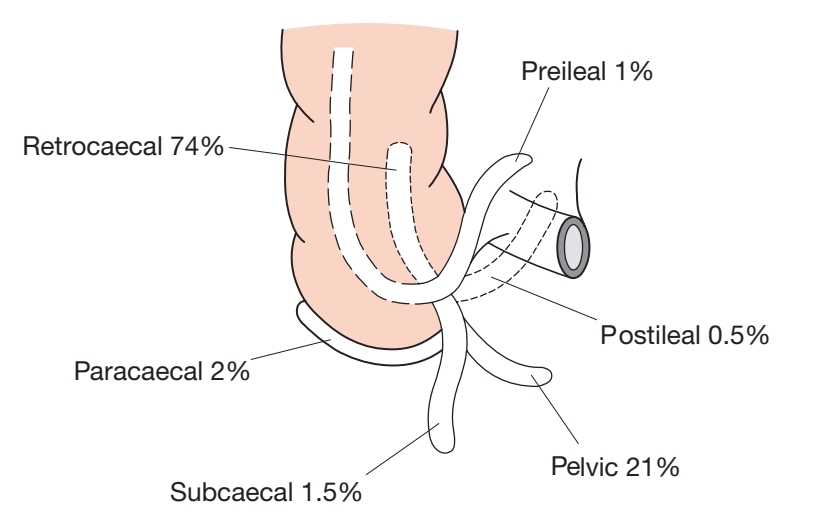
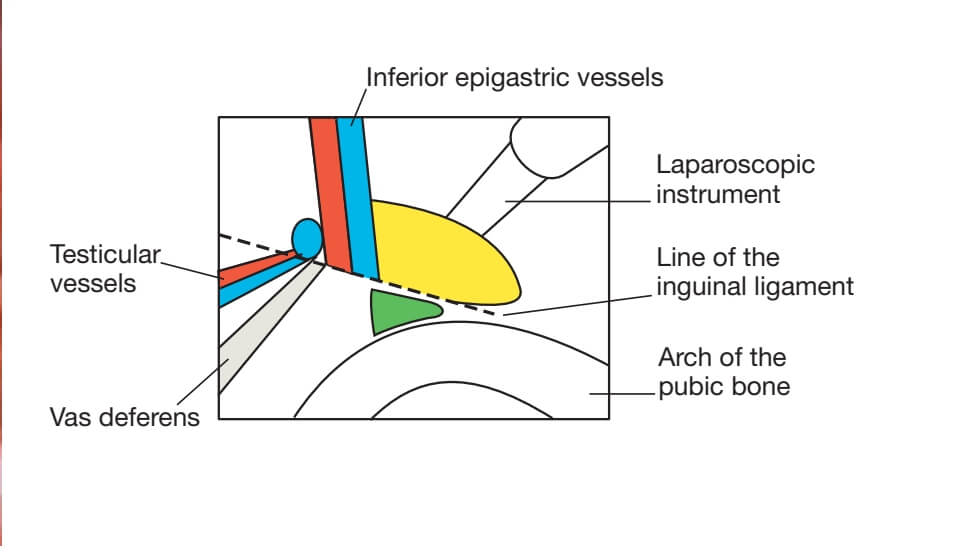
Surgical Anatomy of the Inguinal Region
Inguinal Canal
Length: 4 cm in adults
Location: Parallel and superior to medial half of inguinal ligament
Boundaries:
Anterior wall: External oblique aponeurosis, reinforced laterally by internal oblique
Posterior wall: Transversalis fascia, reinforced medially by conjoint tendon
Roof: Arching fibers of internal oblique and transversus abdominis
Floor: Inguinal ligament and lacunar ligament
Openings of the Inguinal Canal
| Opening | Location | Structures Passing Through |
|---|---|---|
| Deep (Internal) Ring | Midpoint of inguinal ligament, 1.25 cm above | In males: Spermatic cord In females: Round ligament |
| Superficial (External) Ring | Triangular opening in external oblique aponeurosis | In males: Spermatic cord, ilioinguinal nerve In females: Round ligament, ilioinguinal nerve |
Hesselbach’s Triangle
Area of potential weakness in the posterior wall of inguinal canal:
Medial border: Lateral border of rectus abdominis (linea semilunaris)
Lateral border: Inferior epigastric vessels
Inferior border: Inguinal ligament
Clinical significance: Direct hernias protrude through this triangle
Classification of Inguinal Hernias
Anatomical Classification
| Type | Pathway | Incidence | Age Group |
|---|---|---|---|
| Indirect Inguinal | Through deep inguinal ring, along spermatic cord | 65% | All ages (congenital/acquired) |
| Direct Inguinal | Through Hesselbach’s triangle, medial to inferior epigastric vessels | 30% | Middle-aged and elderly |
| Pantaloon Hernia | Combination of direct and indirect components | 5% | Elderly |
Nyhus Classification
| Type | Description | Recommended Repair |
|---|---|---|
| I | Indirect hernia, normal internal ring | Simple closure of neck, high ligation of sac |
| II | Indirect hernia, enlarged internal ring | Closure of internal ring, mesh if large |
| III | A: Direct hernia B: Pantaloon hernia C: Femoral hernia | Mesh repair for all types |
| IV | Recurrent hernia | Mesh repair, consider preperitoneal approach |
Detailed Description of Hernia Types
Indirect Inguinal Hernia
Pathogenesis: Persistence of processus vaginalis (congenital)
Course: Enters deep ring → traverses entire inguinal canal → exits superficial ring
Coverings: Derived from layers of abdominal wall:
External spermatic fascia (from external oblique)
Cremasteric fascia (from internal oblique)
Internal spermatic fascia (from transversalis fascia)
Clinical features: Often descends into scrotum, reduces easily, impulse on coughing
Direct Inguinal Hernia
Pathogenesis: Acquired weakness of posterior wall of inguinal canal
Course: Bulges directly forward through Hesselbach’s triangle
Coverings: Only peritoneum and transversalis fascia (no coverings from cord)
Clinical features: Rarely enters scrotum, wide neck, less risk of strangulation
Clinical Features and Presentation
Symptoms
Groin swelling: Most common presentation, increases with straining
Dragging sensation: Feeling of heaviness or discomfort
Pain: Dull ache that worsens with activity
Asymptomatic: Many hernias are discovered incidentally
Physical Examination Findings
| Examination Technique | Procedure | Findings |
|---|---|---|
| Inspection | Patient standing, coughing | Visible bulge in inguinal region |
| Palpation | Patient supine, reduce hernia then stand | Palpable impulse on coughing |
| Invagination Test | Little finger invaginates scrotum to external ring | Feel impulse at fingertip (indirect) or pulp (direct) |
| Zieman’s Technique | Three-finger examination | Differentiate direct, indirect, and femoral hernias |
Differential Diagnosis
| Condition | Distinguishing Features |
|---|---|
| Femoral Hernia | Below and lateral to pubic tubercle, more common in women |
| Hydrocele | Transilluminates, cannot get above swelling |
| Varicocele | Feels like “bag of worms”, collapses when supine |
| Undescended Testis | Empty scrotum, testis palpable in inguinal canal |
| Lipoma of Cord | Does not reduce completely, no impulse on coughing |
| Inguinal Lymphadenopathy | Firm, non-reducible, multiple nodes possible |
Diagnosis and Investigations
Clinical Diagnosis
According to Love and Bailey, the diagnosis of inguinal hernia is primarily clinical based on:
Thorough history including onset, progression, and symptoms
Careful physical examination in both standing and supine positions
Assessment of reducibility and cough impulse
Examination of contralateral side
Investigations
| Investigation | Indications | Findings |
|---|---|---|
| Ultrasound | Uncertain diagnosis, obese patients, suspected complications | Visualization of hernia sac and contents, differentiation from other masses |
| CT Scan | Complex hernias, recurrent hernias, preoperative planning | Detailed anatomy, size of defect, associated pathologies |
| MRI | Athletes with groin pain, occult hernias | Excellent soft tissue detail, sports hernia diagnosis |
| Herniography | Occult hernia when clinical suspicion high | Contrast outlines peritoneal sac and hernial orifice |
Management of Inguinal Hernia
Conservative Management
Indications:
Asymptomatic or minimally symptomatic hernias
Poor surgical candidates due to comorbidities
Patient preference
Methods:
Watchful waiting with regular follow-up
Truss (rarely used today due to complications)
Lifestyle modifications (weight loss, avoid heavy lifting)
Surgical Management
According to Love and Bailey, surgery is the definitive treatment for symptomatic inguinal hernias.
Open Repair Techniques
| Technique | Principle | Indications | Recurrence Rate |
|---|---|---|---|
| Bassini’s Repair | Approximation of conjoint tendon to inguinal ligament | Historical, rarely used now | 10-15% |
| Shouldice Repair | Four-layer reconstruction with continuous wire suture | Primary hernias in fit patients | 1-2% |
| Lichtenstein Repair | Tension-free mesh repair | Gold standard for open repair | 0.5-1% |
| McVay (Cooper’s ligament) Repair | Conjoint tendon to Cooper’s ligament | Direct hernias with femoral component | 3-5% |
Laparoscopic Repair Techniques
| Technique | Approach | Advantages | Disadvantages |
|---|---|---|---|
| TAPP (Transabdominal Preperitoneal) | Enters peritoneal cavity, then creates preperitoneal space | Good visualization, familiar anatomy | Intraperitoneal access risk |
| TEP (Totally Extraperitoneal) | Enters preperitoneal space directly | Avoids peritoneal cavity, less visceral injury risk | Steep learning curve, limited working space |
Special Considerations
Pediatric Inguinal Hernia
Pathology: Almost always indirect due to patent processus vaginalis
Management: High ligation of sac (herniotomy) without repair of posterior wall
Timing: Elective repair, sooner in infants due to higher incarceration risk
Contralateral exploration: Controversial, considered in infants <2 years
Incarcerated and Strangulated Hernia
Incarceration: Irreducible hernia without vascular compromise
Strangulation: Compromised blood supply to hernia contents
Management: Emergency surgery, bowel resection if necrotic
Mortality: Strangulated hernia has 5-10% mortality rate
Complications of Inguinal Hernia
Complications of Untreated Hernia
| Complication | Incidence | Clinical Features | Management |
|---|---|---|---|
| Incarceration | 5-10% | Irreducible, painful swelling | Attempt manual reduction, surgery if failed |
| Strangulation | 2-3% | Pain, tenderness, signs of obstruction, systemic toxicity | Emergency surgery, resection if bowel necrotic |
| Obstruction | 3-5% | Colicky abdominal pain, vomiting, distension, constipation | NG tube, IV fluids, emergency surgery |
Complications of Hernia Repair
| Complication | Incidence | Risk Factors | Prevention/Management |
|---|---|---|---|
| Recurrence | 1-10% | Direct hernia, large defect, surgeon inexperience, infection | Tension-free mesh repair, proper technique |
| Chronic Pain | 10-15% | Young age, preoperative pain, nerve injury | Nerve identification and preservation, mesh fixation techniques |
| Infection | 1-2% | Diabetes, obesity, hematoma, emergency surgery | Aseptic technique, prophylactic antibiotics |
| Hematoma/Seroma | 5-10% | Anticoagulation, extensive dissection, laparoscopic approach | Meticulous hemostasis, compression, aspiration if large |
| Nerve Injury | 2-5% | Ilioinguinal, iliohypogastric, genitofemoral nerves at risk | Careful identification and preservation of nerves |
| Testicular Complications | 1-2% | Extensive cord dissection, recurrent surgery | Gentle cord handling, preserve testicular vessels |
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Hernias in Love & Bailey’s textbook
European Hernia Society Guidelines
International Guidelines for Groin Hernia Management
Nyhus, L. M., & Condon, R. E. (1995). Hernia (4th ed.). Philadelphia: JB Lippincott.
Key Learning Points from Love & Bailey
“The successful management of inguinal hernia requires thorough knowledge of groin anatomy, careful patient selection, and appropriate choice of surgical technique. Tension-free mesh repair has revolutionized hernia surgery with significantly reduced recurrence rates.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Always examine the patient in both standing and supine positions
Differentiate between direct and indirect hernias clinically when possible
Consider contralateral hernia in pediatric patients
Emergency surgery is mandatory for strangulated hernias
Mesh repair is the gold standard for adult inguinal hernia
Chronic groin pain is the most significant long-term complication
Laparoscopic repair offers advantages for bilateral and recurrent hernias
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog