· Mayank Kashyap · 7 min read
Thyroid gland
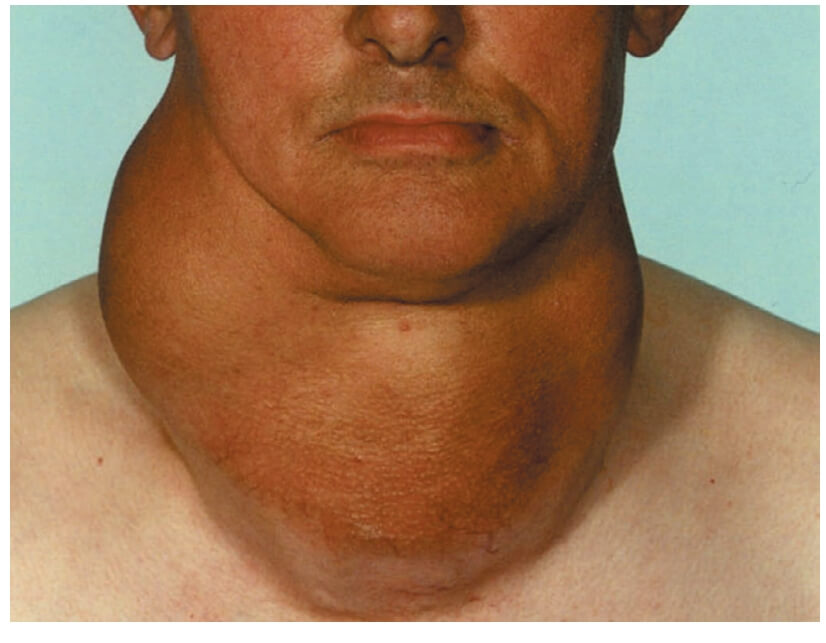
the thyroid gland is one of the most important endocrine organs, regulating metabolism, growth, and development through the production of thyroid hormones.
Anatomy
Thyroid gland is supplied by superior, inferior thyroid and thyroid ima artery.
For the Examination of thyroid gland there are various methods e.g Lahey’s method, Crile’s method, Pizillo’s method.
For thyroid its TIRADS( Thyroid Imaging Reporting and Data System).
There are different types of thyroid surgeries.
Hemithyroidectomy in which 1 lobe and isthmus is removed.
Total thyroidectomy(Removal of whole thyroid gland.)both lobes + isthmus.
Subtotal thyroidectomy Removal of almost all gland and isthmus except
4-8g left on each side.
Near total thyroidectomy
Thyroid cancer includes (Differentiated Thyroid cancer) which includes
Papillary thyroid cancer
Follicular thyroid cancer
Hurthle cell thyroid cancer
Medullary and Anaplastic thyroid cancers.
Causes of hypothyroidism
Iodine deficiency
Hashimoto thyroiditis
Wolf chaikoff effect iodine induced hypothyroidism
Non functioning pituitary adenoma
Sheehan syndrome
Causes of hyperthyroidism
Graves disease
Solitary toxic nodule
Jod basedow phenomenon
TSH secreting pituitary adenoma
Introduction to the Thyroid Gland
According to Love and Bailey’s “A Short Practice of Surgery”, the thyroid gland is one of the most important endocrine organs, regulating metabolism, growth, and development through the production of thyroid hormones.
Embryological Development
Develops from endoderm of primitive pharynx
Appears as an epithelial proliferation in the floor of pharynx
Descends from foramen cecum at tongue base to final position in neck
Thyroglossal duct normally obliterates by 8-10 weeks gestation
Parafollicular C-cells derived from neural crest (ultimobranchial body)
Clinical Significance
Thyroid disorders affect 5-10% of population
More common in females (4:1 female to male ratio)
Goiter prevalence: 4-15% in iodine-deficient areas
Thyroid cancer accounts for 1-2% of all malignancies
Surgical Anatomy of the Thyroid Gland
Gross Anatomy
| Feature | Description |
|---|---|
| Location | Anterior neck, C5-T1 vertebrae level |
| Weight | 15-25 grams in adults |
| Shape | Butterfly-shaped with two lobes and isthmus |
| Dimensions | Each lobe: 5cm height, 3cm width, 2cm thickness |
| Isthmus | Connects lower thirds of lobes, overlies 2nd-4th tracheal rings |
| Pyramidal Lobe | Present in 40-50% of people, remnant of thyroglossal duct |
Capsules of the Thyroid
True Capsule: Peripheral condensation of fibrous stroma
False Capsule: Derived from pretracheal fascia
Surgical Significance:
Vessels run between true and false capsules
Recurrent laryngeal nerve runs outside true capsule
Parathyroids lie between capsules posteriorly
Blood Supply
| Artery | Origin | Course | Clinical Significance |
|---|---|---|---|
| Superior Thyroid Artery | External carotid artery | Descends to upper pole with external laryngeal nerve | Risk of injury to external laryngeal nerve during ligation |
| Inferior Thyroid Artery | Thyrocervical trunk (subclavian) | Ascends posterior to carotid sheath, crosses recurrent laryngeal nerve | Close relationship with recurrent laryngeal nerve |
| Thyroidea Ima Artery | Brachiocephalic trunk or aortic arch | Ascends anterior to trachea to isthmus | Present in 3-10% of people, risk of bleeding during tracheostomy |
Venous Drainage
Superior Thyroid Vein: Drains to internal jugular vein
Middle Thyroid Vein: Directly to internal jugular vein
Inferior Thyroid Veins: Form plexus and drain to brachiocephalic veins
Lymphatic Drainage
Upper pole → Upper deep cervical nodes
Lower pole → Lower deep cervical, pretracheal, paratracheal nodes
Isthmus → Pretracheal and prelaryngeal (Delphian) nodes
Medial portion → Paratracheal nodes
Nerve Supply
| Nerve | Origin | Function | Clinical Significance |
|---|---|---|---|
| Recurrent Laryngeal Nerve | Vagus nerve | Motor to all laryngeal muscles except cricothyroid | Injury causes hoarseness, bilateral injury causes stridor |
| External Laryngeal Nerve | Superior laryngeal nerve (vagus) | Motor to cricothyroid muscle (tensor of vocal cords) | Injury causes voice fatigue, inability to raise pitch |
| Sympathetic Nerves | Superior/middle cervical ganglia | Vasomotor function | No significant surgical implications |
Thyroid Physiology
Thyroid Hormone Synthesis
Iodide Trapping: Active transport into follicular cells
Oxidation: Iodide → Iodine by thyroid peroxidase
Organification: Iodination of tyrosine residues on thyroglobulin
Coupling: MIT + DIT → T3, DIT + DIT → T4
Storage: As colloid in follicular lumen
Release: Endocytosis and proteolysis of thyroglobulin
Thyroid Hormones
| Hormone | Production | Half-life | Biological Activity |
|---|---|---|---|
| T4 (Thyroxine) | 80-100 mcg/day | 7 days | Prohormone, low biological activity |
| T3 (Triiodothyronine) | 20-30 mcg/day | 1 day | Most active form, 3-4x more potent than T4 |
| Reverse T3 | Minor metabolite | 4 hours | Biologically inactive |
| Calcitonin | Parafollicular C-cells | 10 minutes | Calcium homeostasis |
Regulation of Thyroid Function
Hypothalamus: TRH (Thyrotropin-releasing hormone)
Anterior Pituitary: TSH (Thyroid-stimulating hormone)
Thyroid: T4, T3 production
Negative Feedback: T4/T3 inhibit TSH and TRH
Functions of Thyroid Hormones
Metabolism: Increase basal metabolic rate, thermogenesis
Growth & Development: Essential for CNS development in fetus
Cardiovascular: Increase heart rate, cardiac output
Gastrointestinal: Increase gut motility
Neuromuscular: Maintain normal reflex activity
Thyroid Investigations
Thyroid Function Tests
| Test | Normal Range | Clinical Interpretation |
|---|---|---|
| TSH | 0.4-4.0 mIU/L | Most sensitive test for primary thyroid dysfunction |
| Free T4 | 10-25 pmol/L | Measures biologically active thyroid hormone |
| Free T3 | 3.5-7.5 pmol/L | Useful in suspected T3 toxicosis |
| Thyroglobulin | 3-40 ng/mL | Tumor marker for differentiated thyroid cancer |
| Calcitonin | <10 pg/mL | Marker for medullary thyroid carcinoma |
Imaging Studies
| Modality | Indications | Advantages | Limitations |
|---|---|---|---|
| Ultrasound | First-line for thyroid nodules, goiter evaluation | No radiation, excellent resolution, guides FNA | Operator dependent, cannot assess function |
| Radioisotope Scan (Tc-99m, I-123) | Function assessment, toxic nodules, ectopic tissue | Assesses function, whole-body imaging | Radiation exposure, poor anatomical detail |
| CT Scan | Retrosternal extension, lymph node mapping, staging | Excellent anatomical detail, assesses invasion | Radiation, iodine contrast may affect therapy |
| MRI | Soft tissue assessment, recurrent disease | No radiation, excellent soft tissue contrast | Expensive, time-consuming, contraindications |
Fine Needle Aspiration Cytology (FNAC)
| Bethesda Category | Risk of Malignancy | Management |
|---|---|---|
| I: Non-diagnostic | 5-10% | Repeat FNA with ultrasound guidance |
| II: Benign | 0-3% | Clinical follow-up |
| III: Atypia of undetermined significance | 10-30% | Repeat FNA, molecular testing, or surgery |
| IV: Follicular neoplasm | 25-40% | Diagnostic lobectomy |
| V: Suspicious for malignancy | 50-75% | Near-total thyroidectomy or lobectomy |
| VI: Malignant | 97-99% | Definitive surgery |
Benign Thyroid Conditions
Simple Goiter
Definition: Diffuse enlargement without hyperthyroidism
Causes: Iodine deficiency, goitrogens, dyshormonogenesis
Types:
Diffuse hyperplastic goiter (early stage)
Multinodular goiter (late stage)
Management:
Observation if small and asymptomatic
Thyroxine suppression in selected cases
Surgery for pressure symptoms, cosmetic concerns
Toxic Goiter
| Condition | Pathology | Clinical Features | Management |
|---|---|---|---|
| Graves’ Disease | Autoimmune, TSH receptor antibodies | Diffuse goiter, ophthalmopathy, dermopathy | Antithyroid drugs, RAI, surgery |
| Toxic Multinodular Goiter | Multiple autonomous nodules | Older patients, long-standing goiter, cardiac symptoms | RAI or surgery |
| Toxic Adenoma | Single autonomous nodule | Solitary nodule, hyperthyroidism | RAI or surgery |
Thyroiditis
| Type | Pathology | Clinical Course | Treatment |
|---|---|---|---|
| Hashimoto’s Thyroiditis | Autoimmune, lymphocytic infiltration | Progressive hypothyroidism | Thyroxine replacement |
| Subacute (de Quervain’s) Thyroiditis | Viral, granulomatous inflammation | Painful thyroid, transient hyperthyroidism → hypothyroidism | NSAIDs, steroids, beta-blockers |
| Acute Suppurative Thyroiditis | Bacterial infection | Fever, painful swelling, dysphagia | Antibiotics, drainage if abscess |
| Riedel’s Thyroiditis | Fibrous replacement | Hard, fixed goiter, pressure symptoms | Surgery for pressure symptoms |
Thyroid Nodules
Prevalence: 4-7% by palpation, 20-76% by ultrasound
Risk of Malignancy: 5-15% of nodules
Evaluation: TSH, ultrasound, FNA based on size and features
Suspicious Features:
Microcalcifications
Hypoechogenicity
Irregular margins
Taller-than-wide shape
Increased vascularity
Thyroid Malignancies
Classification of Thyroid Cancer
| Type | Frequency | Cell of Origin | Prognosis |
|---|---|---|---|
| Papillary Carcinoma | 80-85% | Follicular cells | Excellent (10-year survival >95%) |
| Follicular Carcinoma | 10-15% | Follicular cells | Good (10-year survival 85%) |
| Medullary Carcinoma | 5-8% | Parafollicular C-cells | Variable (10-year survival 75%) |
| Anaplastic Carcinoma | 1-2% | Follicular cells | Poor (1-year survival 20%) |
| Lymphoma | 1-2% | Lymphocytes | Good with chemotherapy |
Staging of Thyroid Cancer (TNM System)
| Stage | Papillary/Follicular (<45 years) | Papillary/Follicular (≥45 years) | Medullary | Anaplastic |
|---|---|---|---|---|
| I | Any T, Any N, M0 | T1, N0, M0 | T1, N0, M0 | T4a, Any N, M0 |
| II | Any T, Any N, M1 | T2, N0, M0 | T2-3, N0, M0 | T4b, Any N, M0 |
| III | - | T3, N0, M0 or T1-3, N1a, M0 | T1-3, N1a, M0 | Any T, Any N, M1 |
| IVA | - | T4a, Any N, M0 or T1-3, N1b, M0 | T4a, Any N, M0 or T1-3, N1b, M0 | - |
| IVB | - | T4b, Any N, M0 | T4b, Any N, M0 | - |
| IVC | - | Any T, Any N, M1 | Any T, Any N, M1 | - |
Risk Stratification Systems
AMES Classification (for Papillary Cancer)
Low Risk:
All young patients (<41 years)
Older patients with: No distant metastases, Minor extathyroid extension, Primary <5cm
High Risk:
Distant metastases
Major extathyroid extension
Primary >5cm in patients >40 years
MACIS Score (for Papillary Cancer)
Metastasis, Age, Completeness of resection, Invasion, Size
Score <6: 20-year survival 99%
Score 6-6.99: 20-year survival 89%
Score 7-7.99: 20-year survival 56%
Score ≥8: 20-year survival 24%
Thyroid Surgery
Indications for Thyroid Surgery
| Indication | Recommended Procedure |
|---|---|
| Diagnostic uncertainty (suspicious FNA) | Diagnostic lobectomy |
| Confirmed malignancy | Total thyroidectomy ± neck dissection |
| Pressure symptoms (dyspnea, dysphagia) | Total thyroidectomy or subtotal thyroidectomy |
| Cosmetic reasons (large goiter) | Thyroidectomy |
| Hyperthyroidism not controlled medically | Total thyroidectomy or subtotal thyroidectomy |
Surgical Procedures
| Procedure | Description | Indications | Advantages | Disadvantages |
|---|---|---|---|---|
| Hemithyroidectomy (Lobectomy) | Removal of one lobe with isthmus | Diagnostic, benign unilateral disease | Preserves contralateral function, less morbidity | Possible completion thyroidectomy if cancer |
| Total Thyroidectomy | Removal of entire thyroid gland | Malignancy, bilateral disease, Graves’ | Definitive for cancer, no recurrence | Lifelong thyroxine, higher complication risk |
| Subtotal Thyroidectomy | Removal of most thyroid tissue, leaving small remnants | Benign multinodular goiter, Graves’ disease | May preserve thyroid function | Risk of recurrence, difficult reoperation |
| Near-total Thyroidectomy | Removal of all tissue except small posterior remnant | Differentiated thyroid cancer | Lower complication rate than total | Small risk of recurrence in remnant |
Surgical Complications
| Complication | Incidence | Prevention | Management |
|---|---|---|---|
| Recurrent Laryngeal Nerve Injury | 1-2% (permanent), 3-5% (temporary) | Identification and preservation of nerve | Voice therapy, medialization procedures |
| Hypoparathyroidism | 1-3% (permanent), 10-20% (temporary) | Identification and preservation with blood supply | Calcium and vitamin D supplementation |
| Hemorrhage/Hematoma | 1-2% | Meticulous hemostasis, drain if large dead space | Emergency evacuation if airway compromise |
| Infection | <1% | Aseptic technique | Antibiotics, drainage if abscess |
| Hypothyroidism | 100% after total thyroidectomy | N/A | Lifelong thyroxine replacement |
| Keloid/Hypertrophic Scar | 5-15% | Careful skin closure, anatomical lines | Steroid injections, scar revision |
Postoperative Management
Immediate:
Monitor for bleeding, respiratory distress
Check serum calcium at 6-12 hours postop
Voice assessment
Short-term:
Thyroid function tests at 4-6 weeks
Start thyroxine replacement if total thyroidectomy
Wound check at 1-2 weeks
Long-term (for cancer):
Radioactive iodine ablation if indicated
Thyroglobulin monitoring
Neck ultrasound surveillance
TSH suppression therapy
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Thyroid and Parathyroid Surgery in Love & Bailey’s textbook
American Thyroid Association Guidelines
British Thyroid Association Guidelines
American Association of Clinical Endocrinologists Guidelines
Key Learning Points from Love & Bailey
“Thyroid surgery requires meticulous technique with thorough knowledge of anatomy, particularly the relationship of the recurrent laryngeal nerve and parathyroid glands. The choice of surgical procedure should be tailored to the specific pathology and patient factors.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
All thyroid nodules require evaluation with TSH and ultrasound
FNAC is the cornerstone of thyroid nodule evaluation
Recurrent laryngeal nerve identification is mandatory in thyroid surgery
Parathyroid glands should be identified and preserved with their blood supply
Most thyroid cancers have excellent prognosis with appropriate treatment
Postoperative calcium monitoring is essential after total thyroidectomy
Multidisciplinary approach is crucial for thyroid cancer management
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog